
As the data collection methods have extreme influence over the validity of the research outcomes, it is considered as the crucial aspect of the studies
May 2025 | Source: News-Medical
The healthcare sector is going through digital transformation and Artificial Intelligence (AI) is the primary agent of change. AI technologies which are being applied in healthcare require substantial amounts of high-quality data to be reliable and efficient. Two of the largest sources of data for AI in healthcare are Electronic Health Records (EHRs) and Patient-Reported Outcomes (PROs) obtained from wearables. Employing these data sources is allowing organizations to better the quality of patient care and improve decision-making and overall management and operation.
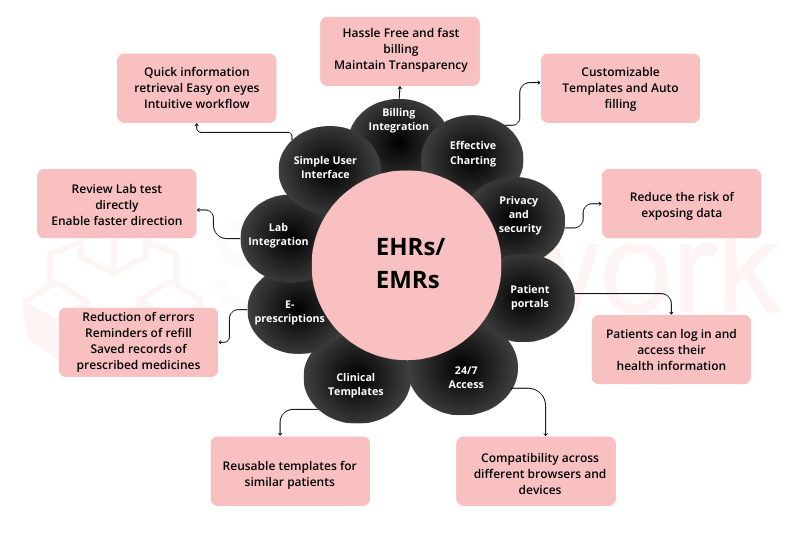
EMRs and EHRs are electronic accounts of a patient’s medical history that are kept by a health care provider. They typically include diagnoses, treatment plans, medications, laboratory results, and patient demographic information. Since EHRs are automatically updated at every visit, they provide real-time, structured data that will be required to create AI healthcare models. [1]
Overview:
Patient-reported outcomes (PROs) are types of health data provided directly by the patient as self-reports of symptoms, satisfaction with treatments, and the quality of life. Additionally, wearable devices (e.g., fitness trackers) and medical grade sensors that collect real time data are a new source of health care data that include physical activity, heart rates, and sleep. PROs and other patient-centered data is an important source of data for artificial intelligence (AI) health care solutions seeking to customize patient care.[5]
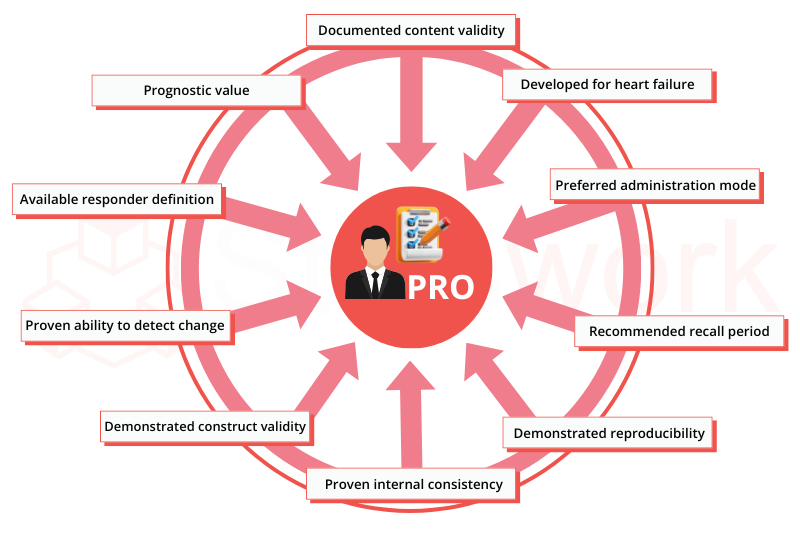
AI-driven healthcare applications rely on the health data — diverse and plentiful — to improve the quality of care and predict health outcomes. Electronic Health Records (EHRs) provide many insights into a patient’s clinical status while Patient-Reported Outcomes (PROs) can provide real-time data collection from wearable devices with a patient-centric approach. Together, these forms of data allow AI to augment decision making, personalizing care, and providing better health outcomes.
For an organization considering using AI solutions, data security, privacy, and interoperability are vital issues. Without interoperability it will be hard to create AI ecosystems with integrated data collection that advance equitable effective care.
Are You Ready to Use AI for Health Innovation?
At Statswork, we help healthcare organizations—both public and private—leverage AI with advanced data analytics. By leveraging electronic health records (EHRs), patient-reported outcomes (PROs), and wearable data, we facilitate the creation of intelligent, efficient healthcare applications that revolutionize patient care and operational performance.
WhatsApp us